What is CLL/SLL?
You may have recently learned that you, or someone you love, have been diagnosed with cancer called chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). You may have been told that you have both diseases at the same time. You may be looking for more information about these diagnoses and what to expect.
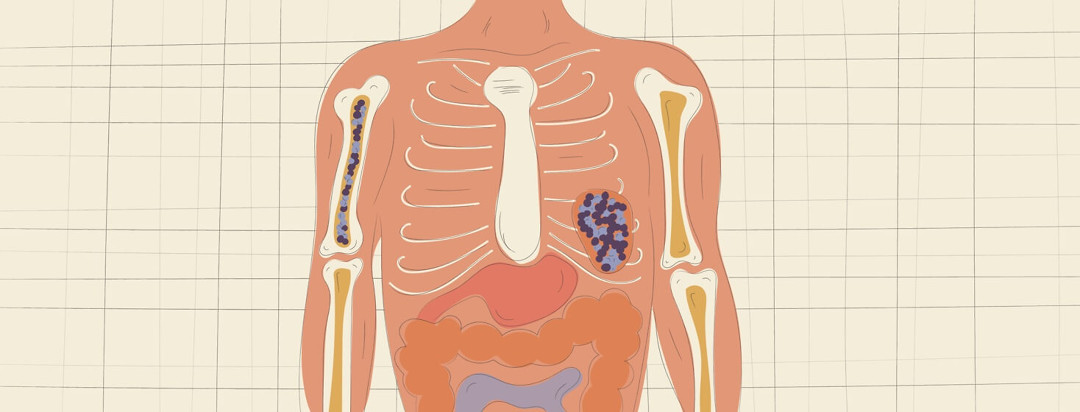
As your doctor may have explained, CLL and SLL are cancers of a certain type of blood cell, called a “lymphocyte.” CLL/SLL falls under the category of non-Hodgkin lymphoma, and it is specific to your B-lymphocytes (also referred to as “B cells”).1 These diseases are often grouped together because they tend to happen concurrently, however there are differences between the two diagnoses, and you can have either one without having the other. The main difference between the two is that CLL is a cancer that affects B-cells that are in the blood and bone marrow, while SLL is the same cancer but it affects B-cells in the lymph nodes and/or the spleen.1
Featured Forum
View all responsesWho gets chronic lymphocytic leukemia?
CLL/SLL is more common in older patients (the average age of diagnosis is 65, but it can happen in younger and older patients), and generally is more common in men than in women.2 Many patients can have CLL/SLL and not realize it until they have routine blood work or a physical; these patients may not have symptoms for many years.1 Symptoms that some patients do notice include: swollen lymph nodes, feeling extremely tired, notice that they are short of breath easily, noticing that they may bruise easily, they may have drenching night sweats, weight loss, or may notice swelling in their belly, and feel full easily.1,2
Chronic lymphocytic leukemia stages
Your doctor will run tests on your CLL/SLL to tell you what stage your disease is. Your doctor may run a test called a FISH test to understand the specific genetics of your disease. This will help them decide how to treat your cancer.
CLL is often staged using the Rai Staging System which is staged by risk.3
- Low-risk CLL has a high lymphocyte count in the blood and bone marrow.
- Intermediate-risk CLL has a high lymphocyte count and enlarged lymph nodes or enlarged liver/spleen.
- High-risk CLL has a high lymphocyte count and either anemia (low hemoglobin, which carries oxygen in the blood) or low platelet count (platelets are the part of the blood which makes you clot).
SLL is often staged using the Ann Arbor Staging Method, which is staged by disease progression.4
- Stage I is when only one set of lymph nodes is involved.
- Stage II is when 2 or more sets of lymph nodes are involved but they are all in the chest/neck or abdomen.
- Stage III is when 2 or more sets of lymph nodes are involved in both the chest and abdomen.
- Stage IV is when Multiple lymph nodes and organs are involved and the disease is widespread.
How does staging help?
Staging helps your doctor decide what the best treatment option is for your disease. Many CLL/SLL patients have “Indolent disease”.1,3 This means that their disease is kept in check by their immune system, so there is no need for treatment. Most of these patients don’t exhibit symptoms of CLL/SLL or if they have symptoms, they are very mild. These patients are treated using the “watch and wait” method. Patients will see their Oncologist every few months to be examined or have blood tests run to see how their disease is progressing. If their blood counts change, their lymph nodes increase in size (this may be referred to by your doctor as “lymphadenopathy”) or if they start exhibiting symptoms that their disease is progressing, their doctor may suggest starting treatment.3
How is chronic lymphocytic leukemia treated?
If your doctor tells you that your disease has progressed, they may discuss treatment options with you. There are currently three main treatment options for CLL/SLL. Chemotherapy, which is drugs that target and kill cancer cells, can be given in a pill form, or as an injectable. Targeted therapies are drugs that target specific parts of the cancer cell, and can be both in a pill form or an injectable.
Lastly, there are monoclonal antibodies, which are antibodies that are grown in a lab to attach to specific parts of the cancer cell causing it to die. Monoclonal antibodies are almost always injectable medications. Many times these types of drugs are often given in combinations to treat CLL/SLL.3 There are many new drugs being researched for CLL/SLL currently; new therapies are regularly being approved, so make sure you discuss therapy options with your doctor. There are also clinical trials available for patients who may have run out of standard treatment options. Your care team can help you find a clinical trial if you want to participate in one.1
Talk to your care team about any questions you may have about your diagnosis and what it means for you. Be sure to let them know about concerns you have about your disease, about tests results you don’t understand, and about your treatment. Your care team will work to find the best treatment plan for you and your specific diagnosis.
Community Poll
Have you taken our In America Survey yet?
Join the conversation