What Is Chronic Myeloid Leukemia (CML)?
Reviewed by: HU Medical Review Board | Last reviewed: June 2024 | Last updated: June 2024
Blood cancers generally affect the process of making new blood cells, resulting in unhealthy levels of blood cells. Chronic myeloid leukemia (CML) is a type of blood cancer in which the body creates too many abnormal white blood cells.1
New blood cells are made from blood stem cells. These are usually found in the bone marrow, the spongy center of the bones. A blood stem cell can become a myeloid stem cell or a lymphoid stem cell.1,2
Usually, myeloid stem cells can become red blood cells, white blood cells, or platelets. But CML causes many of the myeloid stem cells to become unhealthy white blood cells. This can result in having fewer healthy white blood cells, red blood cells, and platelets.1,2
What causes CML?
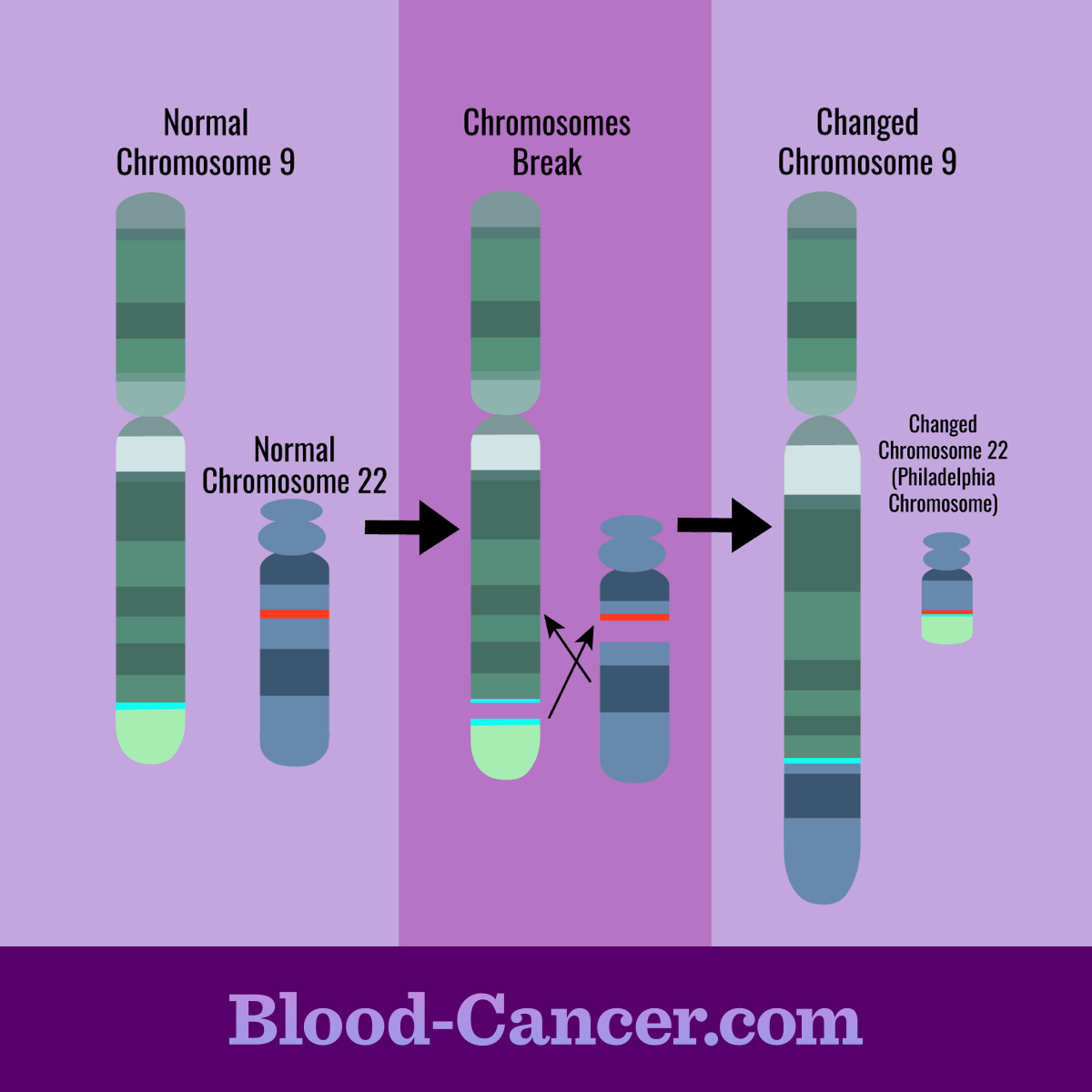
CML is caused by a change in a person’s DNA. Each cell in your body has a copy of the DNA, which is normally packed into 46 chromosomes. CML often occurs when a section of chromosome 22 switches with a section of chromosome 9.1
This switch causes the bone marrow to produce a protein that increases the number of abnormal white blood cells. The new mixed chromosome 22 is called the “Philadelphia chromosome,” which is present in most cases of CML.1
Figure 1. Philadelphia chromosome
Risk factors for developing CML
Experts know of only a few factors that can increase a person’s risk for CML. They are:2
- Exposure to high doses of radiation – This would include a nuclear reactor accident or atomic bomb blast.
- Age – The risk increases as people get older.
- Gender – The risk is slightly higher for men than for women.
Symptoms of CML
Some people do not experience symptoms of CML in the beginning. They may find out they have CML during routine blood tests. In people who do have symptoms, their symptoms may include:1,3
- Fatigue, weakness, or tiredness
- Weight loss
- Fever
- Night sweats
- Headaches
- Bone pain
- Bleeding
- Infections
- Swollen lymph nodes
- Anemia (lack of healthy red blood cells)
CML also can cause the spleen to grow larger, which can lead to symptoms such as:1,3
- A sense of fullness in the belly
- Feeling full after only eating a small amount of food
How is CML diagnosed?
Doctors typically diagnose CML with several tests, including a blood test called complete blood count (CBC) with differential. This test measures the number of red blood cells, platelets, and different types of white blood cells in your blood.1
Along with blood tests, your doctor also will do a physical exam. The most common physical sign of CML is an enlarged spleen. During the physical exam, your doctor may use their fingers to feel whether the spleen is larger than normal. Your doctor may also do a bone marrow biopsy for more advanced tests.1,3
Phases of CML
CML is grouped into 3 phases generally based on the amount of immature white blood cells (also called blast cells) found in your blood.1,3,4
- Chronic phase – In this phase, blast cells make up less than 10 percent of total blood cells. People may experience few or no symptoms during this phase.1,3,4
- Accelerated phase – In this phase, blast cells make up 10 to less than 20 percent of total blood cells. More symptoms typically start to appear during this phase.1,3,4
- Blast phase – In this phase, blast cells make up at least 20 percent of total blood cells. The blast cells may have spread to other tissues. At this stage, CML tends to behave like acute leukemia.1,3,4
Treatment and outlook for CML
Tyrosine kinase inhibitors (TKIs) are one form of treatment available for CML. These prescription drugs are usually used during the chronic phase of CML, but some also may be used during accelerated and blast phases. Examples of TKIs include:1,3
- Imatinib (Gleevec®)
- Bosutinib (Bosulif®)
- Dasatinib (Sprycel®)
- Nilotinib (Tasigna®)
- Ponatinib (Iclusig®)
- Asciminib (Scemblix®)
This or That
Are you or a loved on living with leukemia?
Your doctor will monitor how well the treatment is working with regular blood tests. Some people may not respond to a certain TKI. In this case, your doctor may suggest switching to a different TKI.3
Over the past few decades, the survival rate for CML has improved greatly. The overall 5-year survival rate for CML is 70 percent. Researchers also are testing new drugs and treatments, which could further improve the survival rate.5